Understanding the “FVRCP” vaccine & “modified live-virus” vaccines!

What is the “FVRCP” vaccine?
The FVRCP vaccination is an important part of your cat’s routine.
It prevents three potentially deadly airborne viruses:
- rhinotracheitis
- calicivirus
- panleukopenia
- Rhinotracheitis is triggered by the common feline herpes virus. Symptoms include sneezing, a runny nose and drooling. Your cat’s eyes may become crusted with mucous, and he or she may sleep much more and eat much less than normal. If left untreated this disease causes dehydration, starvation, and eventually, death.
- Calicivirus has similar symptoms, affecting the respiratory system and also causing ulcers in the mouth. It can result in pneumonia if left untreated—kittens and senior cats are especially vulnerable.
- Panleukopenia is also known as distemper and is easily spread from one cat to another. Distemper is so common that nearly all cats—regardless of breed or living conditions—will be exposed to it in their lifetime. It’s especially common in kittens who have not yet been vaccinated against it, and symptoms include fever, vomiting and bloody diarrhea. This disease progresses rapidly and requires immediate medical attention. Without intervention, a cat can die within 12 hours of contracting the disease.
These three viruses can be contracted by cats at any age.
Kittens should receive their first FVRCP vaccination at 6 to 8 weeks of age, followed by three booster shots once a month. Adult cats should receive a booster once every year or two, according to your veterinarian’s recommendation.
Adult cats with unknown vaccination records should receive a FVRCP vaccination, plus a booster in 3-4 weeks from the time they initially received the first FVRCP vaccine.
Because FVRCP is a live vaccine, it should not be given to pregnant cats. If a live-vaccine is administered to a pregnant cat then the unborn kittens may develop cerebellar hypoplasia.
What is a “modified- live” vaccine?
Modified live vaccines (MLV) contain a small quantity. of virus or bacteria that has been altered so that it no longer. is capable of causing clinical disease but is still capable of. infection and multiplying in the animal.
What is the difference between the various types of vaccines?
There are three major types of vaccine:
1. Modified live vaccines. These vaccines contain live organisms that are weakened or genetically modified so that they will not produce disease but will multiply in the cat’s body. Live vaccines induce a stronger, longer lasting immunity than inactivated vaccines. It is not advisable to use modified live vaccines in pregnant queens or cats whose immune system is not working properly (e.g., cats infected by feline immunodeficiency virus (FIV), or other diseases).
2. Killed (inactivated) vaccines. These vaccines are prepared using actual organisms or genetically modified organisms that have been killed by various treatments. On their own, they do not give as high a level of protection as the live, replicating type of vaccine, so killed vaccines may have an adjuvant (an added ingredient) to make the immune response stronger.
3. Subunit vaccines. These are more commonly called recombinant-DNA vaccines. These are vaccines in which the infectious organism has been broken apart and only certain parts are included in the vaccine.
How do vaccines work exactly?
Vaccines work by stimulating the body’s immune system to recognize and fight a particular microorganism such as a virus, bacteria, or other infectious organism. Once vaccinated, the animal’s immune system is then primed, or prepared to react to a future infection with that microorganism. In other words, the vaccine mimics a true infection so that the immune system can better protect the body in the future. Depending on the disease, the vaccine will help the body prevent infection or lessen the severity of infection and promote rapid recovery.
Which particular brand of the FVRCP vaccine is considered “modified-live”?
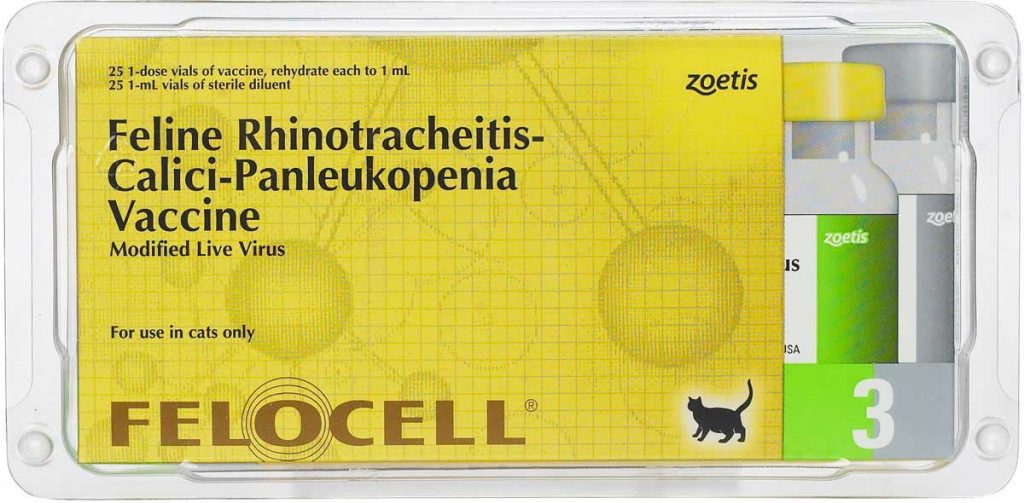
- FELOCELL (Zoetis)
- FELOCELL 3 is a non-adjuvanted* modified-live virus (MLV) vaccine.
- Contains attenuated strains of feline rhinotracheitis virus, calicivirus, and panleukopenia virus (Johnson Snow Leopard strain), propagated on established cell lines.
- Safety of FELOCELL 3 was demonstrated in field trials involving 2,288 cats. No serious post-vaccination reactions attributable to the vaccine were reported.
- Packaged in freeze-dried form with inert gas in place of vacuum.
- Customer-friendly packaging includes peel-off labels for faster and more accurate record-keeping, a color-coded organizing system, and an easy-open safety band.
- FELOCELL 3 is supported by our Companion Animal Immunization Support Guarantee (ISG).
* Non-Adjuvanted : An adjuvant is a substance that is added to a vaccine to enhance the body’s immune response to the vaccine. Studies have shown that adjuvants have been associated with injection site reaction, injection site granuloma, and chronic inflammation in cats. (purevax.com)
The AAFP vaccination guidelines recommend that low-risk adult cats be vaccinated every three years for the core vaccines, and then as determined by your veterinarian for any non-core vaccines. Some vaccine manufacturers have developed approved three-year vaccines for many of the core vaccines. It is important to note that feline leukemia virus (FeLV) vaccine is recommended by some AAFP members as a core vaccine, while other experts classify it as a non-core vaccine. Your veterinarian is the ultimate authority on how your cat should be vaccinated. Please always consult your cat’s veterinarian about the vaccine schedule/process, types of vaccines, side effects & more!















